As a human being, you probably like to think you are totally in control of your own body.
How it functions and how you think and feel but actually, the truth of the matter is quite different.
You are made up of less than 1% human DNA!
The rest of you is teeming with microbes which number in their trillions – a rich soup of bacteria, fungi, viruses and protozoa to name just a few…..
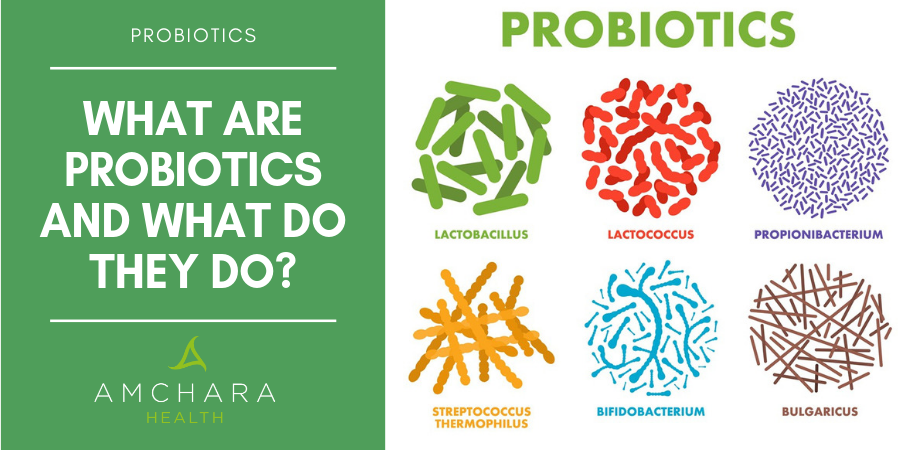
Live Bacteria
By definition, live or healthy bacteria – also known as probiotics are living micro-organisms that can alter the host microflora and exert specific health benefits without increasing the risk of antibiotic resistance.
These minute organisms — or most of them at least — are commensal, which means they live happily alongside us and are essential for our survival, not to mention our continuing health and wellbeing.
It’s quite amazing that we have such a limited understanding of our tiny fellow inhabitants but that’s mostly to do with their size, the complexity of their functions and because they are hidden so deeply within us.
Bacteria like to live in areas of the body that provide suitable conditions for them to grow and proliferate, like the warm moist areas of our skin folds.
The upper respiratory airways and genital tract also harbour bacteria, however, the greatest numbers of bacteria are found in the digestive tract – the mouth, stomach and intestines.
The gastrointestinal tract is the natural habitat for a large and dynamic bacterial community, which is colonised from birth when we begin to develop a highly complex ecosystem of micro-organisms.
Babies are born with a sterile intestinal tract but rapidly acquire micro-biota which amazingly develops into a microbiome totally unique to any other humans.
The microflora of a baby’s intestines resembles that of the adult’s flora following weaning.
The establishment of the gut microbial population is a rather complex process influenced not just by the mother but also by environmental factors such as hospitalisation, hygienic conditions and antimicrobial procedures.
Lactobacilli and bifidobacteria will establish itself in new-borns that are breast fed due to the presence of oligosaccharides and prebiotic factors in breast milk.
In addition bifidus factor, lactoferrin casein and nucleotides will promote an increase in the colonisation of these bacteria.
On the other hand, babies fed with cow’s milk formula, will develop mainly enterobacteria and gram-negative organisms.
This is because of the absence of the prebiotics’ variables contained in human milk and the alkaline milieu.
It may also be that external influences post-delivery are more important in gut colonisation than breast-feeding.
The microbiota comprises mainly bacteria; however, this extends to viruses, fungi and protozoans.
Our microbiota contains trillions of bacterial cells, 10 times more cells than the number of cells that make up the human body.
These micro-organisms have many major functions some of which are still relatively unknown.
Prebiotics play an equally important role in gut health but these are different from probiotics.
Compared with probiotics, which introduce external bacteria into the human colon, prebiotics are non-digestible food ingredients that stimulate the preferential growth of a limited number of health-promoting flora already living in the colon; especially, but not exclusively, lactobacilli and bifidobacteria.
Prebiotics are found naturally in fruit and vegetables such as:
- Apples
- Bananas
- Asparagus
- Onions
- Leeks
- Jerusalem artichoke
- Chicory
- Legumes
- Beans
- Garlic
- Sweet potato
- Squash
- Carrots
- Beetroot
- Cabbage
Combinations of probiotics and prebiotics are called synbiotics.
These work together in a synergistic way more efficiently promoting the benefits of probiotics.
The Origins of Probiotics
The word probiotic is derived from the Greek meaning for ‘life’.
The history of probiotics parallels the evolution of the human race and thanks to modern technology can be traced back to ancient times.
Long before people were aware of probiotic microorganisms, the diets of many populations included fermented products such as bread, cheese yoghurt and kefir.
It’s likely that the first foods that contained living microorganisms were the fermented milk that are recorded in the Old Testament.
Fermented products were probably discovered quite by accident; for example, yoghurt may have been produced as a result of transportation methods, whereby animal skins bags were used to carry milk and water in low humidity and high temperatures.
The consumption of fermented milk in various different forms has continued until the present day.
Functions of the Gut Flora
The whole concept of helpful or ‘friendly’ bacteria may seem confusing since bacteria are usually associated with diseases and illnesses.
Nevertheless, fermented milk containing the strains Streptococcus thermophilus and Lactobacillus bulgaricusin have been ingested by humans for thousands of years in the belief that they have health benefits.
In more recent history ‘probiotics’ in the form of probiotic bacteria are becoming increasingly important in the context of human nutrition, as research evidence continues to accumulate on the properties, benefits and functionality, of probiotics for the promotion of human health.
The gut flora comprises an amazing 95% of the total number of cells in our bodies (100,000 billion organisms).
As an adult, we’re estimated to be carrying around more than 1,000 species, but maybe even as many as 40,000, from more than 7000 different strains, so it’s not surprising that there’s a lot we still don’t know about what goes on in this vast microbial ecosystem.
What we do know is that the gut micro flora has a profound influence on our health at multiple levels.
Gut microorganisms use the vegetables and fruit that we eat to regulate many critical functions which include not just our immune systems, but our appetites, brain function and the way we use energy.
It has been suggested that probiotics can play an important role in digestive and respiratory functions as well as immunity and could have a significant effect on alleviating infectious diseases in children.
The metabolic functions of the gut flora are numerous and include:
- Digestive function through enzyme activity.Maintenance of appropriate gut pH
- Production of lactase production of natural antimicrobial substances, in order to defend against invaders, prevent the growth of pathogens and maintain a healthy balance of microfloraBreak down of bacterial toxins
- Helps to normalise serum cholesterol and triglycerides – Live bacteria are able to convert cholesterol into a less absorbable form leading to reduced absorption of cholesterol from the gastrointestinal tract therefore a fall in serum cholesterol levels
- Mineral absorption
- Bio transforms plant polysaccharides
- Regulates immune function
- Synthesizes vitamins.
- Bifidobacteria can produce a range of vitamins including folic acid, vitamin B1, B6, B12, and vitamin K, as well as a variety of amino acids.
- Releases plant polyphenols
- Produces short chain fatty acids to provide energy to the epithelial cells and throughout the body.
- Detoxifies many substances
- Regulates peristalsis and bowel movements
- Produces natural antimicrobials helping to prevent growth of pathogens.
A Balancing Act
The gut microflora are generally stable which is due to regulation of the ecosystem by competition for space, nutrients, inhibition etc.
However, if this balancing act is disturbed it is possible for inflammation and disease to occur due to an overgrowth of pathogenic organisms and increased stimulation of the immune system.
The stability of the gut flora can be affected by a variety of factors and these include:
- Antibiotic therapy – antibiotics have a detrimental effect not just on the unhealthy pathogenic bacteria but also on the beneficial bacteria which may leave the gut open to eventual invasion by further opportunistic pathogens.
- Stress and trauma – General stress, as well as specific incidences of trauma, affect the fine balance of the microbial flora in a harmful manner. Stress decreased gastric and intestinal secretions leading to an increase in the intestinal pH and a concomitant reduction in gut motility. This results in a more favourable environment for the growth of more opportunistic pathogens such as Streptococci and E.coli and a less favourable environment for slower growing beneficial bacteria like lactobacilli and Bifidobacteria
- Nutrition – The introduction of the modern western diet, high in processed and refined foods, has led to a decrease in consumption of beneficial micro-organisms. And this appears to affect the equilibrium of the gastrointestinal microflora. Normal microflora balance can be re-established once the adverse influences causing an abnormal distribution of gut microbes are eliminated. The most effective way to do this is to encourage an increase in the growth of lactobacilli and Bifido by consuming foods with live bacteria or taking supplements.
Choosing the Right Strain
As many as 400 different types of organisms have been isolated from the gut.
However, a lot of these are only found occasionally or are found in very small numbers.
The bulk of the population of the microbiota is comprised of several types of bacteria which must be able to survive the hostile acidic environment of the stomach and be resistant to bile salts and intestinal secretions.
Increasing evidence has shown the critical role played by the microflora in everyday well-being.
Hence there is growing interest in the use of probiotic preparations to supplement the diet.
As scientific research has advanced, it has become apparent that specific characteristics are desirable in probiotics and that there are also potential shortfalls associated with some.
It is believed by many that the ideal probiotic should remain viable at the level of the intestine and should be able to adhere to the intestinal epithelium and establish itself in the human gut in order to confer a significant health benefit.
Some research evidence suggests that viable bacteria are associated with having greater immunologic effects than nonviable bacteria and that the death of some bacteria leads to adverse effects in some instances.
Most probiotics with beneficial properties are strains of Bifidobacterium or Lactobacillus species and some of these exhibit powerful anti-inflammatory activities.
Some are derived from the intestinal microbiota of healthy humans, and others are non-human strains used in the fermentation of dairy products.
Species from other bacterial genera such as Streptococcus, Bacillus, and Enterococcus have also been used as probiotics, but there are concerns surrounding the safety of such probiotics because these genera contain many pathogenic species particularly Enterococcus.
Non-bacterial microorganisms such as yeasts from the genus Saccaromyces have also been used as probiotics for many years.
In summary, criteria considered important when selecting probiotic strains include:
- Organisms that are of human origin
- Organisms should be non-pathogenic
- Organisms need to be bile tolerant
- Organisms should be able to adhere to the gut epithelial tissue
- Organisms must be genetically stable
- Organisms should be able to produce antimicrobial substances
- Organisms should be able to inhibit pathogens
- Organisms should exert a positive effect on certain metabolic pathways
- Organisms should be able to retain viability during manufacturing processes and delivery mechanisms in the body
- Organisms should have proven clinical research to support their use
Risks
Given the increasingly widespread use of probiotics by both health practitioners and the general public, clinicians need to have an understanding of the risks associated with probiotic treatments and must be aware that there is uncertainty regarding their use in some areas.
The highest area of concern for probiotic use is the risk of sepsis.
There have been some reports linking cases of Lactobacillus and other bacterial cases of sepsis with the ingestion of probiotic supplements.
However, in all cases, these have occurred in patients with underlying compromised immunity, debilitation and chronic disease.
There have been no adverse reports relating to the use of probiotics in otherwise healthy individuals.
Apart from some rare instances, the majority of probiotic sepsis have been resolved with the appropriate use of antimicrobials.
According to the World Health Organization (WHO) working together with the Food and Agriculture Organization (FAO) ‘theoretically’ probiotics may be responsible for four possible side effects:
- Deletrious metabolic activities
- Gene transfer
- Systemic infections
- Excessive immune stimulation in susceptible individuals.
The WHO/FAO working group, recommend more research on new probiotic strains to evaluate their safety and efficacy by testing for antibiotic resistance, haemolytic potential, metabolic activities and toxin production.
Clinical Uses
The popularity in the use of live bacteria in the form of probiotic supplementation is growing hugely, largely due to increasingly rigorous scientific evaluation in recent years.
There is now strong evidence to support their numerous health benefits.
Perhaps the most compelling evidence for probiotic efficacy is in relation to the anti-diarrheal effects and helping to regulate bowel movements.
It is well documented that the use of antibiotics disturbs the balance of gut flora and can result in complications such as diarrhoea, gastritis and an overgrowth of Candida.
A research review carried out in 2002 revealed that administering live bacteria following antibiotic therapy could reduce the associated diarrhoea and prevent multiplication of Candida albicans.
In 2010 The American Journal of Gastroenterology reported that administering a blend of lactobacillus acidophilus and lactobacillus casei resulted in a reduced risk of antibiotic-associated diarrhoea and clostridium difficile associated diarrhoea.
An earlier study by Cheng et al in 2005 demonstrated that the use of both lactobacillus acidophilus and bifidobacteria bifidum following antibiotic therapy resulted in a significant reduction of opportunistic pathogen re-growth.
Irritable bowel syndrome (IBS) is a common complaint where friendly bacteria are thought to exert a beneficial effect.
The culprit for IBS is thought to be a bacterial overgrowth in the small intestines, so repopulating the gut with healthy bacteria may play a role in alleviating the symptoms.
Promising studies appear to support this theory.
In particular, one large-scale trial carried out in 2006 assessed the efficacy of Bifidobacterium infantis on women with IBS.
Results from this research revealed a significant improvement in abdominal discomfort, wind and incomplete evacuation compared to those in the placebo group.
Inflammatory Bowel diseases such as Crohn’s and Ulcerative Colitis may also benefit from the use of friendly bacteria.
Research suggests that certain pathogenic bacteria present in the GI tract may aggravate these conditions.
Healthy bacteria influences the balance of the gut flora so may be helpful for IBD sufferers.
Research News
It seems that the gut micro flora may also be implicated in insulin sensitivity and obesity related disorders.
Research is now recognising that pre-biotics and friendly bacteria might have beneficial effects on glucose tolerance, post-prandial insulin release and insulin sensitivity.
A Finnish study carried out in 2009 on 256 pregnant women, identified that the group taking Lactobacillus rhamnosus GG & Bifidobacterium lactis Bb12 alongside nutrition counselling had better glucose tolerance with higher insulin sensitivity than the placebo group.
It was found that 18% fewer women given the live bacteria had central obesity.
They also had an average body fat of 28% compared to 29-30% in the placebo group.
This study provided evidence of consistently improved glucose metabolism due to combined dietary counselling and live bacteria supplementation.
Exciting new research is also proposing that manipulation of the colonic micro biota improves chronic fatigue symptoms.
In addition to this, a growing body of research is showing the health benefits of taking mixed strains of live bacteria.
A study in The Journal of Gastroenterology Hepatology in 2013 found favourable results for using a multi strain probiotic for those with IBS.
The use of Bifidobacterium longum, Bifidobacterium bifidum, Bifidobacterium lactis, Lactobacillus acidophilus, Lactobacillus rhamnosus and Streptococcus thermophilus gave substantial relief from symptoms such as pain, discomfort and bloating compared to no change in the placebo group.
This trial also highlighted the need for using live bacteria rather than functional foods such as yogurt drinks, which a previous study had found to be ineffective.
What is also interesting in relation to IBS is the improvement in levels of depression that has been found by sufferers who were taking probiotics to improve their gut symptoms.
Valuable new research published in the medical journal Gastroenterology in 2017, found that double the number of participants with IBS reported improvements from co-existing depressive conditions when they took a particular probiotic than the adults with IBS that took a placebo.
Researchers are also exploring the links between thyroid health and the gut flora.
Scientists have learnt that 80% of the immune system’s response to the environment is induced by bacterial ecosystems, which means that a healthy gut microbiota could have a significant effect on the body’s immunity.
Given that as many as 90% of hyperthyroid disorders have an autoimmune component it seems likely that it is triggered by an imbalance of bacteria in the gut. (1)
The Bottom Line
Interest in the use of live bacteria within the food industry, from consumers and particularly within the scientific community is growing.
Although benefits vary, depending on the type and amount of probiotic consumed, experts in the health industry agree that daily consumption of foods containing these beneficial components is a necessary addition to a balanced healthy diet.
It should be noted that the effects of probiotics are strain specific and this must be demonstrated through appropriate trials.
It is anticipated that further scientific investigations into this expanding area may uncover even more insights into the beneficial role of friendly bacteria.
Jacqueline Newson BSc (Hons) Nutritional Therapy
READ THIS NEXT:
- Probiotics – Another Tool to Enhance your Weight-Loss Programme
- Probiotics offer relief for IBS
- Good health starts in the gut
- The Gut: the centre of your health?
- Is my gut in balance?